Abstract
The position of the condyle can be determined using different diagnostic tools, among which are transcranial X-rays (RT), Cone Beam Computed Tomography (CBCT), and the Condylar Position Indicator (CPI). This study aimed to determine the concordance among the CPI, the CBCT, and the RT as diagnostic methods for determining the condyle position. Materials and method: 32 valid cases, each of which had an RT, a CBCT, and a CPI, were analyzed by three observers. SPSS V. 26.0 program was used to calculate the Kappa trust interval, using the jackknife technique which allows to estimate of the standard error between observers. To evaluate the condylar position using CPI, an AD2 articulator was employed. A Pullinger and Hollender layout was used in the tomographic and transcranial images. Results: The concordance among the three observers for each method resulted in a value of Kappa higher than 0.879. The concordance between CBCT and RT was 0.0627, between CPI and RT it was 0.247, and between CBCT and CPI it was .188. Conclusion: The level of concordance obtained between the three observers with any given diagnostic method was very good, which indicates that the concordance that each observer obtained regarding each diagnostic method is trustworthy. In this study, it is concluded that there is a concordance in the diagnosis regarding the position of the condyle of the tomography with the transcranial radiography. There is no concordance between tomography and CPI. There was also no concordance between the CPI and the transcranial radiography.
Highlights
- The position of the condyle can be determined using different diagnostic tools.
- The level of agreement obtained between the three observers with any diagnostic method was very good, therefore, it is reliable.
- The position of the mandibular condyle differed significantly in the methods studied, thus suggesting that the actual position of the condyle requires imaging.
1. Introduction
It has been suggested that the condylar position may be related to dysfunctions of the gnathic system [1]. The condylar position may have a dramatic effect on the position of the mandibular body, which, in turn, may significantly affect the diagnosis and treatment in diverse areas of dentistry [2]. The size and position of mandibular condyles among different sagittal skeletal relationships [3]. Several types of X-rays have been used to identify this position and the Transcranial projection was the first to be used [4]. However, said images were difficult to interpret due to anatomical reasons. Laminographic research and research using tomography led to the conclusion that the precision of the images could be improved by orienting the ray of the X-rays along the condylar axis, determined by a sub-vertex. Still, tomographic studies of normal samples showed an ample variety of condylar positions, and for this reason, didn’t provide clinically useful information [5]. The Condylar Position Indicator (CPI) allows us to measure the vertical, transversal, and anteroposterior deviations of the condyle. This can be used to evaluate the condylar position in the diagnostic and treatment plan for the patients [6]. There aren’t any publications that study the trustworthiness or exactitude of this registry; a specific study about this diagnostic method would be required for that. The Cone Beam Computed Tomography (CBCT) is a 3D imaging technique that is precise, economical, and exposes patients to a relatively low amount of radiation. CBCT is amply used in treatments that involve the maxillofacial region, and it is also the method of choice for determining bone changes in the condyle, and position changes in the spaces of the temporomandibular articulation. Although images obtained through magnetic resonance are considered the gold standard in isolating soft tissues, CBCT provides better images with better information regarding the state of the articulations and bone changes [7].
2. Materials and methods
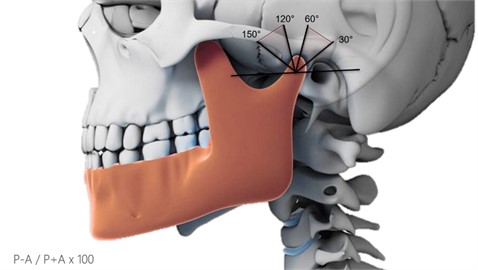
A total of 16 subjects (32 mandibular condyles) were included in the study. It should be noted that the patient’s personal information was treated as confidential and that the ethical principles established in the Helsinki Declaration were respected at all times. Transcranial X-rays, CBCT, and CPI were obtained for each patient. The transcranial X-rays and the CBCTs were taken at the same radiological center, and all of them were measured and analyzed following the guidelines of Andrew Pullinger and Lars Hollender [8]. The three studies were measured by three observers, trained to be able to carry out and interpret the measurements of the three different diagnostic methods. The position of the middle point of the condyle was determined, and an angle conveyor was employed in such a way that its base coincided with a line drawn from Petro’s tympanic fissure to the lowest point of the articular tubercle. The anteroposterior position of the angle conveyor was defined as the perpendicular line that traversed the middle point of the condyle. The inter-articular distances were measured linearly in 30°, 60°, 120° and 150° angles. The area of the posterior space was comprised between 30° and 60°, and the area of the anterior space was between 120° and 150°. The averages of both zones were divided among each other, following the formula of posterior space / anterior space x 100, where 0 was the condylar center; values of less than -12 represented a posterior position, and values of more than 12 represented an anterior position (Fig. 1). Cast models were used to obtain the registry of the condyle's position through CPI. The bite was registered using pink wax in a central occlusion. The models were mounted on an AD2 articulator, as seen in Fig. 2. The Kappa index was used to determine the level of concordance among the observers in all the different diagnostic methods. This index was also used to determine the correlation between the different diagnostic methods, based on their concordance, to establish the position of the mandibular condyle, using a SPSS V. 26.0 program.
Fig. 1Method established by Pullinger and Lars Hollender, used to determine the position of the condyle in transcranial X-rays and tomography
3. Results
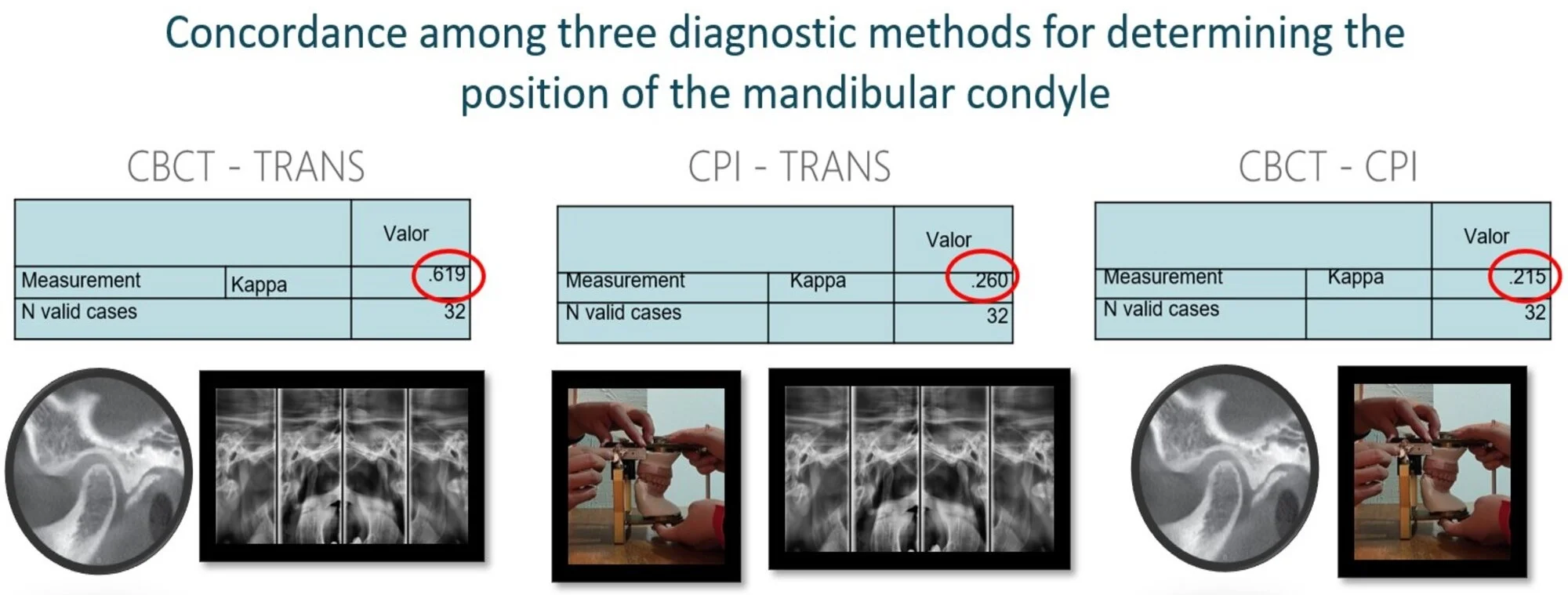
All measurements were carried out by three observers for all three of the diagnostic methods. The Kappa analysis shows the level of concordance among the different diagnostic methods. It should be noted that the highest level of concordance was found between the CBCT and trans-cranial X-ray methods and was established at 0.631 (Table 1). On the other hand, the lowest level of concordance was found between CBCT and CPI at 0.175 (Table 2). Finally, the level of concordance between trans-cranial X-rays and CPI was 0.221 (Table 3).
Fig. 2Method used to mount the models on an AD2 articulator and thus obtain the position of the mandibular condyle
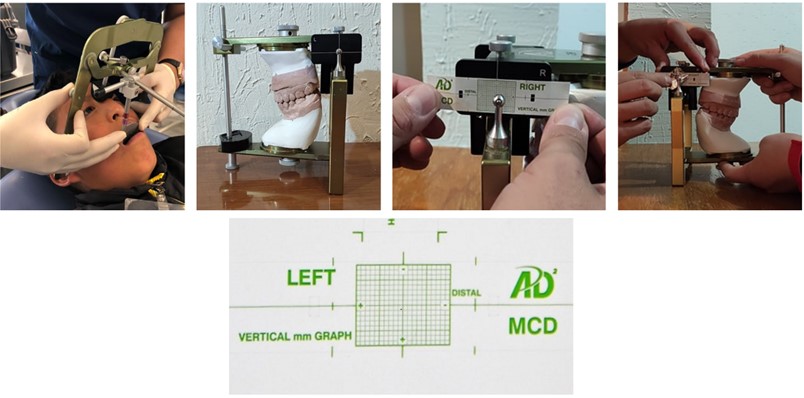
Table 1Value of the Kappa analysis between CBCT and trans-cranial x-ray
Value | Standard asymptotic errora | Approx. Sb | Approx. Sig. | ||
Measurement | Kappa | 0.631 | 0.137 | 3.934 | 0.000 |
N valid cases | 32 | ||||
The value obtained was 0.631 which indicates that the level of correlation between CBCT and trans-cranial X-rays was good.
Table 2Value of the Kappa analysis between CBCT and CPI
Value | Standard asymptotic errora | Approx. Sb | Approx. Sig. | ||
Measurement | Kappa | 0.175 | 0.149 | 1.219 | 0.223 |
N valid cases | 32 | ||||
The value of Kappa was determined to be 0.175, which indicates a low level of correlation between CPI and CBCT.
Table 3Value of the Kappa analysis between CPI and trans-cranial x-ray
Value | Standard asymptotic errora | Approx. Sb | Approx. Sig. | ||
Measurement | Kappa | 0.221 | 0.141 | 1.590 | 0.112 |
N valid cases | 32 | ||||
The value obtained was 0.221 which indicates that the level of correlation between CPI and trans-cranial X-ray is low.
As one can observe, the results were very similar for all observers about the values of Kappa obtained. The highest degree of correlation was always obtained between measurements taken using CBCT and trans-cranial X-rays. The lowest degree of correlation was obtained between measurements taken using CBCT and CPI. The level of correlation between measurements taken using CPI and trans-cranial X-rays was a little higher than those obtained using CBCT and CPI, but those were also consistently low. Table 4 shows the concordance levels obtained by the three observers using CBCT, and Table 5, shows the concordance levels obtained by the three observers using trans-cranial X-rays. The concordance levels obtained by the three observers using CPI are observed in Table 6.
Table 4Value of the Kappa analysis between the different observers using the CBCT measurements
Value | Standard asymptotic errora | Approx. Sb | Approx. Sig. | ||
Measurement | Kappa | 0.935 | 0.064 | 5.821 | 0.000 |
N valid cases | 32 | ||||
The value obtained was 0.935, which indicates that the level of correlation among the observers was very good.
Table 5Value of the Kappa analysis between the different observers using trans-cranial x-rays. d
Value | Standard asymptotic errora | Approx. Sb | Approx. Sig. | ||
Measurement | Kappa | 0.879 | 0.083 | 5.427 | 0.000 |
N valid cases | 32 | ||||
The value obtained was 0.879, which indicates that the level of correlation among the observers was very good.
Table 6Value of the Kappa analysis between the different observers using CPI
Value | Standard asymptotic errora | Approx. Sb | Approx. Sig. | ||
Measurement | Kappa | 1.000 | .000 | 7.195 | .000 |
N valid cases | 32 | ||||
The value obtained was 1, which indicates that the level of correlation among the observers was near perfect.
As one can observe, the degree of concordance among the observers to determine the position of the condyle using any single method was always very good, which allows us to conclude that the correlations obtained (both high and low) between the different methods have a high degree of trustworthiness.
4. Discussion
The position of the condyle can be determined using different methods, some of which are very specialized and sophisticated, while others are simpler. Some examples of methods are the trans-cranial X-ray, CBCT, and CPI, among others. This study is interested in determining the level of concordance between these methods because each one of them has specific advantages over the others in terms of their efficacy in determining the position of the condyle. No previous studies had been conducted to allow us to determine the level of concordance between the tools for making diagnostics which may allow us to determine which diagnostic method to use at a given moment.
First, it’s worth noting that the observers who participated in this study displayed a high level of concordance regarding Kappa for all diagnostic methods used, which suggests that this study can be replicated. If one observes Tables 4 and 5, regarding the position of the condyle within the glenoid cavity, the most frequent position of the condyle determined with all three diagnostic methods was a centric condylar position. The anterior condylar position was the second most frequent, and the posterior condylar position was the least frequent. This tendency was concordant among the three observers.
In a study conducted by Alexander et al. (1993), to observe the condylar position in Centric Occlusion, and the posterior position with regards to the position of the median articular disc, with an articulator and magnetic resonance, the researchers found that said methods were reproducible, but only one researcher was in charge of all the measurements. This was not the case in the present study, in which three observers replicated the observations [9].
Presently it hasn’t been possible to reach a consensus among different authors to determine a possible physiological position of the condyles inside the glenoid cavity. Some studies suggest that the position of the condyle outside of the concentricity would be related to malocclusions [10] or the presence of temporomandibular dysfunction [11], [12] but not all authors agree upon this point [13].
In a study conducted by Alves et al. (2014), in which the condylar position and the articular space were evaluated, it was determined that most of the subjects studied had their condyles located in the posterior condylar position (39.47 %), followed by concentric position (34.21 %), and anterior position (26.31 %) [14]. These results do not coincide with our study in which the most frequent condylar position was that of concentricity. The concordance obtained according to the Kappa analysis of the measurements taken by observer 1 among the different methods was 0.175 between CPI and CBCT, 0.221 between CPI and transcranial X-rays, and 0.631 between transcranial X-rays and CBCT, which suggests that the correlation between CPI and CBCT is weak, as is also the case between CPI and transcranial X-rays; none the less, the concordance between CBCT and trans-cranial x-rays was good. The results obtained by observer 2 were similar to those of observer 1, and the concordances obtained using the Kappa analysis were as follows: 0.215 between CPI and CBCT, 0.260 between CPI and trans-cranial x-rays, and 0.619 between CBCT and transcranial X-rays, which corroborates the poor concordance in the first two cases, and a good concordance in the third case. Observer 3 registered values very similar to those registered by his colleagues. The concordances obtained by observer 3 using the Kappa analysis were as follows: 0.175 between CPI and CBCT, 0.341 between CPI and trans-cranial X-rays, and 0.631 between CBCT and trans-cranial X-rays. As was also the case with observers 1 and 2, observer 3 registered a poor concordance in the first two cases, and a good concordance in the third case. Additionally, it is worth mentioning that the three observers who participated in this study evidenced a high level of Kappa concordance in all the diagnostic methods analyzed, which shows that the study can be replicated (see Tables 4, 5, and 6).
The concordance among the three observers was measured using the same method, and the concordance values when evaluating CBCT were 1, 0.935, and 0.935 between observers 1 and 3, 1 and 2, and 2 and 3 respectively. The concordance values obtained for trans-cranial X-rays were 0.935, 0.879, and 0.879 between observers 1 and 3, 1 and 2, and 2 and 3 respectively. Finally, the values obtained when analyzing concordance among observers for CPI were 1 for all three observers. This indicates that the existing concordance among observers for any given diagnostic method is very good. This also suggests that the results are trustworthy and that the concordance between diagnostic methods is likely valid.
Lars Hollender and Andrew Pullinger (1985) conducted a study that concluded that in 80 % of the X-rays analyzed there existed a qualitative concordance of the position of the condyle, whether it was evaluated in a posterior manner, concentrically, or anteriorly [8]. This suggests that transcranial X-rays may have clinical uses. Nonetheless, the 60 % rate of complete concordance and the apparent tendency of trans-cranial X-rays to exaggerate non-concentricity in 30 % of cases, led Lars Hollender and Andrew Pullinger to prefer tomography as their diagnostic method of choice.
Menezes et al., (2008) conducted a study in which the position of the mandibular condyle determined using trans-cranial X-rays and magnetic resonances was compared. Magnetic resonance is considered the gold standard for measuring changes in the position of the mandibular condyle and visualizing inter-articular spaces [15]. Their study showed that there was no significant difference between the results obtained using trans-cranial X-rays, and magnetic resonance. This coincides with the results of the present study since the Kappa values obtained while evaluating concordance among the three observers show that the study is reproducible (the values of Kappa were between 0.69 and 0.91). In their study, Menezes et al. concluded that trans-cranial X-rays are an acceptable method, the applicability of which, as a complementary method, should not be discarded. Even when the method used in the present study isn’t the same as that used by Menezes et al. in 2008, we coincide with their results in terms of not having found significative differences between tomography and transcranial X-rays, and with regards to the concordance among observers, which allowed us to conclude that our study was reproducible and that there exists concordance between the two diagnostic methods.
Ikeda and Kawamura (2009) conducted a study of tomography in which they measured the distance of the articular space in patients without temporomandibular dysfunction [16]. The researchers found no difference between the subjects in terms of gender, and the measurements were very similar, which indicates a concentric position of the condyle. The researchers suggested that their measurements should be taken into account and used as the norm for clinical measurements that attempt to determine the position of the condyle within the glenoid cavity. Additionally, their conclusions coincide with the more recent study conducted by Guerrero Aguilar Andrea Victoria (2017). Nonetheless, we consider these studies to be flawed because they didn’t use multiple observers. Although the measurements carried out by Ikeda and Kawamura were performed on tomography, we consider that they could also be performed using transcranial X-rays, since our present study shows that there exists concordance and reproducibility.
Even when the objective of the present study is not to determine whether the condylar position influences the criteria for a diagnosis of temporomandibular dysfunction, we agree that the condylar position as a means for diagnosis is very weak [17], since there are many factors involved in the diagnostic. Nonetheless, it is of great importance to determine beforehand whether the elements used for a diagnostic are trustworthy or not. Also, the different elements used for a diagnostic offer a series of cost-benefit advantages and disadvantages for the patient which need to be taken into account.
Currently, there exists a great interest in determining the condylar position and understanding its association with temporomandibular disorders, thus many studies have been conducted that research the relationship between the condylar position and the presence of temporomandibular dysfunctions. For these studies, many different methods have been used, such as the one devised by Guimarães and colleagues in 2017 which uses tomography [18]. Guimarães and colleagues reported that there was no correlation between the condylar position and temporomandibular disorders. In a different study, they used CPI to determine the condylar position. The same as with the 2017 study, a single researcher set up the articulator to determine the position of the condyle within the glenoid cavity. In the beforementioned studies, there was no possibility of comparing concordance between observers or establishing whether it was reproducible or not since this diagnostic method requires not only a specific amount of time for the set-up but also the clinical registry [2].
In 2003, Lavine and colleagues carried out a study to measure the reproducibility of CPI, in which the registries were done by three operators [6]. The authors showed that the measurements of the three different operators were very precise and very similar to one another. These results coincide with our own because, in the current study, a very high level of concordance among the observers was found, which allows us to say there is trustworthiness and consistency. Other authors, were also interested in the relationship between the condylar position determined through the measurement of spaces within the glenoid cavity, and its relation to the cranial index and the presence of temporomandibular dysfunctions [19]. The researchers analyzed said position with sonographic registries and didn’t find any differences among the subjects of the study. On the other hand, an ample bibliographical review was carried out, and few studies included this diagnostic method. A study was recently published in which they compared the mandibular condyle position used resonance compared to the CPI. They concluded that the position of the mandibular condyle differed significantly thus suggesting that the real position of the condyle requires imaging [20]. We agree with the aforementioned since the CPI did not show concordance in the condyle position concerning the tomography and transcranial X-rays. In the present study, the concordance levels obtained between CPI and two other diagnostic methods were weak, and we could observe that transcranial X-rays have a good concordance with tomography and that being cheaper than tomography, can be used as a reliable method for determining the position of the condyle.
5. Conclusions
The level of concordance obtained between the three observers with any given diagnostic method was very good, which indicates that the concordance that each observer obtained regarding each diagnostic method is trustworthy. In this study, it is concluded that there is a concordance in the diagnosis regarding the position of the condyle of the tomography with the transcranial radiography. There is no concordance between tomography and CPI. There was also no concordance between the CPI and the transcranial radiography.
References
-
W. Chow, Z. He, Y. Liu, J. Song, C. Xu, and E. Luo, “Intraoperative condylar positioning techniques on mandible in orthognathic surgery,” Orthodontics and Craniofacial Research, Vol. 25, No. 4, pp. 449–458, Nov. 2022, https://doi.org/10.1111/ocr.12568
-
S. Padmanabhan, S. Padala, and A. Chithranjan, “Comparative evaluation of condylar position in symptomatic (TMJ dysfunction) and asymptomatic individuals,” Indian Journal of Dental Research, Vol. 23, No. 1, p. 122, 2012, https://doi.org/10.4103/0970-9290.99060
-
J. A. Tariq Qua, “Condylar size and position, comparison among different sagittal skeletal relationships: A CBCT Study,” Journal of the College of Physicians and Surgeons Pakistan, Vol. 33, No. 5, pp. 509–515, May 2023, https://doi.org/10.29271/jcpsp.2023.05.509
-
K. L. Knoernschild, S. A. Aquilino, and A. Ruprecht, “Transcranial radiography and linear tomography: a comparative study,” The Journal of Prosthetic Dentistry, Vol. 66, No. 2, pp. 239–250, Aug. 1991, https://doi.org/10.1016/s0022-3913(05)80055-1
-
K. Ikeda, A. Kawamura, and R. Ikeda, “Assessment of optimal condylar position in the coronal and axial planes with limited cone-beam computed tomography,” Journal of Prosthodontics, Vol. 20, No. 6, pp. 432–438, Aug. 2011, https://doi.org/10.1111/j.1532-849x.2011.00730.x
-
D. Lavine, R. Kulbersh, P. Bonner, and F. E. Pink, “Reproducibility of the condylar position indicator,” Seminars in Orthodontics, Vol. 9, No. 2, pp. 96–101, Jun. 2003, https://doi.org/10.1053/sodo.2003.34030
-
Y.-I. Kim, B.-H. Cho, Y.-H. Jung, W.-S. Son, and S.-B. Park, “Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: Le Fort I osteotomy and mandibular setback surgery with rigid fixation,” Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, Vol. 111, No. 6, pp. 681–687, Jun. 2011, https://doi.org/10.1016/j.tripleo.2010.08.001
-
A. Pullinger and L. Hollender, “Assessment of mandibular condyle position: A comparison of transcranial radiographs and linear tomograms,” Oral Surgery, Oral Medicine, Oral Pathology, Vol. 60, No. 3, pp. 329–334, Sep. 1985, https://doi.org/10.1016/0030-4220(85)90319-6
-
S. R. Alexander, R. N. Moore, and L. M. Dubois, “Mandibular condyle position: Comparison of articulator mountings and magnetic resonance imaging,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 104, No. 3, pp. 230–239, Sep. 1993, https://doi.org/10.1016/s0889-5406(05)81724-x
-
V. R. Ganugapanta, “Computed tomographic evaluation of condylar symmetry and condyle-fossa relationship of the temporomandibular joint in subjects with normal occlusion and malocclusion: a comparative study,” Journal of Clinical and Diagnostic Research, Vol. 11, No. 2, 2017, https://doi.org/10.7860/jcdr/2017/21678.9328
-
C.-X. Li et al., “A pilot investigation of condylar position and asymmetry in patients with unilateral posterior scissors-bite malocclusion based on three-dimensional reconstructive imaging technique,” BMC Musculoskeletal Disorders, Vol. 24, No. 1, pp. 1–11, Apr. 2023, https://doi.org/10.1186/s12891-023-06384-z
-
J. M. Barrera-Mora et al., “The relationship between malocclusion, benign joint hypermobility syndrome, condylar position and TMD symptoms,” CRANIO®, Vol. 30, No. 2, pp. 121–130, Apr. 2012, https://doi.org/10.1179/crn.2012.018
-
Bulmario Gonzalez, “The not-so-controversial issue of condylar position,” International Journal of Orthodontics (Milwaukee, Wis.), Vol. 18, No. 2, pp. 17–26, 2007.
-
N. Alves, N. F. Deana, Q. A. Schilling, V. A. González, L. J. Schilling, and R. C. Pastenes, “Evaluación de la Posición Condilary del Espacio Articular en ATM de Individuos Chilenos con Trastornos Temporomandibulares,” International Journal of Morphology, Vol. 32, No. 1, pp. 32–35, Mar. 2014, https://doi.org/10.4067/s0717-95022014000100006
-
A. V. Menezes, S. M. de Almeida, F. N. Bóscolo, F. Haiter-Neto, G. M. B. Ambrosano, and F. R. Manzi, “Comparison of transcranial radiograph and magnetic resonance imaging in the evaluation of mandibular condyle position,” Dentomaxillofacial Radiology, Vol. 37, No. 5, pp. 293–299, Jul. 2008, https://doi.org/10.1259/dmfr/31850388
-
K. Ikeda and A. Kawamura, “Assessment of optimal condylar position with limited cone-beam computed tomography,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 135, No. 4, pp. 495–501, Apr. 2009, https://doi.org/10.1016/j.ajodo.2007.05.021
-
N. D. Mohl, “Reliability and validity of diagnostic modalities for temporomandibular disorders,” Advances in Dental Research, Vol. 7, No. 2, pp. 113–119, Aug. 1993, https://doi.org/10.1177/08959374930070020101
-
F. Vale, I. Francisco, A. Guimarães, M. Lopes, A. Lucas, and F. Caramelo, “Condylar form alteration on skeletal class II patients that underwent orthognathic surgery: an overview of systematic reviews,” Journal of Clinical and Experimental Dentistry, Vol. 12, No. 7, pp. e695–e703, 2020, https://doi.org/10.4317/jced.56947
-
L. Pereira, M. Gavião, L. Bonjardim, and P. Castelo, “Ultrasound and tomographic evaluation of temporomandibular joints in adolescents with and without signs and symptoms of temporomandibular disorders: a pilot study,” Dentomaxillofacial Radiology, Vol. 36, No. 7, pp. 402–408, Oct. 2007, https://doi.org/10.1259/dmfr/16641858
-
J. Freudenthaler, S. Lettner, A. Gahleitner, E. Jonke, and A. Čelar, “Static mandibular condyle positions studied by MRI and condylar position indicator,” Scientific Reports, Vol. 12, No. 1, pp. 1–9, Oct. 2022, https://doi.org/10.1038/s41598-022-22745-5
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Aidé Terán Alcocer: Participation in conceptualization, an observer making the measurements in the three diagnostic elements; project administration, investigation, resources, writing original draft, preparation, review, and editing. Alejandro Liévano Ruíz: Participation in conceptualization, and investigation; as an observer making the measurements in the three diagnostic elements and formal analysis. Elia Irene Núñez Hernández: Participation as an observer making the measurements in the three diagnostic elements. Héctor Ernesto Ruíz Valdez: Participation in data curation. Alejandro Lloret Rivas: Participation in Methodology and Redaction. Claudia Verónica Cabeza: Participation in clinical administration. Miguel Francisco Javier Lloret Rivas: Participation in project administration, resources, supervision, visualization, writing original draft preparation, review, and editing.
The authors declare that they have no conflict of interest.
All subjects signed informed consent. The personal information was treated as confidential and that the ethical principles established in the Helsinki Declaration were respected at all times.
