Abstract
This case report intends to present a functional appliance designed by the first author, that follow the principles expected for all functional appliances. It is not anchored on teeth. It does not produce mechanical forces and uses tongue and mandible posture change as natural forces. The appliance was used for 24 months, only to sleep. The patient came complaining discomfort with improper occlusion of the teeth and temporomandibular pain. Body balance was evaluated by DIERS and was also altered. It was possible to find out the presence of a unilateral crossbite and alteration on condyle position inside the cavity evaluated by CBCT. After the treatment with CPB (Cranial Posture Balance) appliance associated with osteopathic procedures, the occlusion and the temporomandibular complains were improved.
Highlights
- Cranial Posture Balance CPB is a new jaw functional orthopedics appliance
- CPB improved occlusal balance in na adult patient
- CPB associated to osteopathic treatment improves the body posture of the patient
1. Introduction
Functional orthopedics for adults focuses on addressing the musculoskeletal system, including bones, muscles, joints, ligaments, and tendons, to improve function and overall well-being. It involves identifying and correcting underlying issues that contribute to chronic pain or limitations, with an interdisciplinary approach that considers the interconnection of body systems [1-3]. Functional orthopedic appliances (FOA) can be used since temporary dentition until mature permanent dentition [1]. Its main characteristic is not to act through mechanical forces but instead to generate remodeling stimuli through changes in tongue and jaw posture [4]. The creation of a device that can simplify the reposition the jaw and restore the correct position of the tongue, acting in an adult mouth, opens up therapeutic possibilities that are still little used. This work proposes an approach that combines a new FOA and manual therapy to re-establish the mandible and tongue position, as well as the consequent bone remodeling and postural balance.
2. Case report
A 36-year-old man with unilateral crossbite (Fig. 1) and facial asymmetry in addition to joint discomfort underwent dental and osteopathic evaluation. The determination of a treatment plan and selection of medical approaches were based on a comprehensive examination, including functional evaluations, analysis of plaster models of dental arches, cone beam computed tomography (CBCT), and also manual and visual testing using the “from bite to foot” method [5], created by the first author (appendix). After diagnosis, the patient underwent to an osteopathic manual therapy to liberate fascia, associated to the use of the CPB [6] to posture the mandible in a correct position and guide the tongue for the palate (Fig. 2). The CPB was constructed to maintain the mandible in a manipulated position avoiding dental interferences. The Coffin was constructed with the curvature to the front and anteriorized to allow bigger stimulation of the premolar and canine area. The appliance was used 12 hours a day, always including sleeping time and the activation was done every 15 days.
Fig. 1Beginning pictures: a) inclined view to show the negative overjet on posterior right, characterizing unilateral crossbite and generating midline deviation to the right; b) frontal view showing that in the manipulated position, avoiding dental interferences, the midline is almost centralized indicating that crossbite and deviation were positional due to narrowing of the palate requiring remodeling on both sides
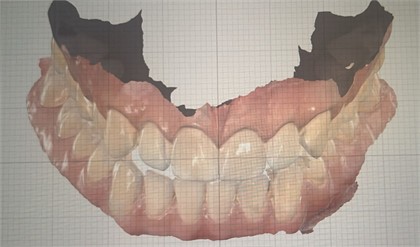
a)
b)
Fig. 2a) Design of the CPB: 1 – coffin spring, that can be constructed with the curvature for anterior or posterior, depending on the necessity of each case, the position in the palate can also vary depending on the transversal gain necessity; 2 – acrilic internal shield, 3 – posterior stabilizer, 4 – anterior stabilizer, 5 – curved wave bar to guide the position of the tongue, it can come from superior down if the tongue is pressuring more superior and can come from inferior up if the tongue is pressuring more inferior; b) real model of CPB
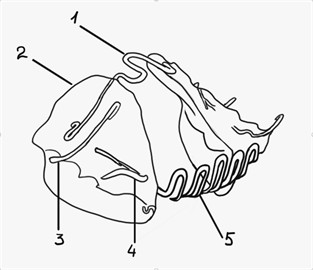
a)
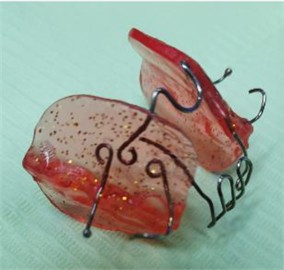
b)
3. Results
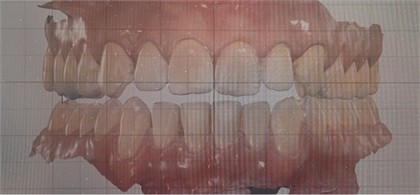
After 24 months, the patient occlusion was regularized with centralized mandibular midline.
The appliance generated remodeling on maxillae and mandible even without mechanical forces (Fig. 3). The presence of the acrylic touching the palate generated remodeling on transversal direction. Each fifteen days the acrylic was adjusted together with the Coffin. The tongue pressure on Coffin also act as a stimulus to enhance palatal transversal remodeling.
Fig. 3CBCT 3D reconstruction showing the effect of the therapeutic. Merged image shows the high level of remodeling on right side
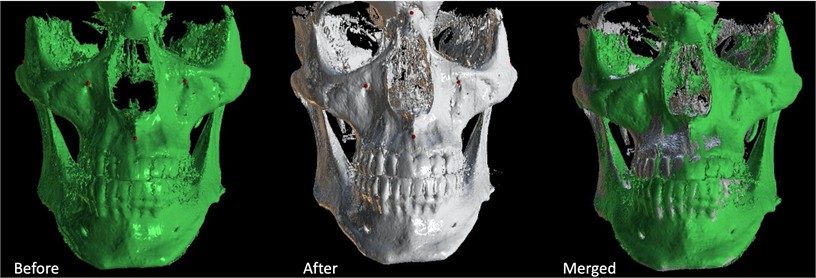
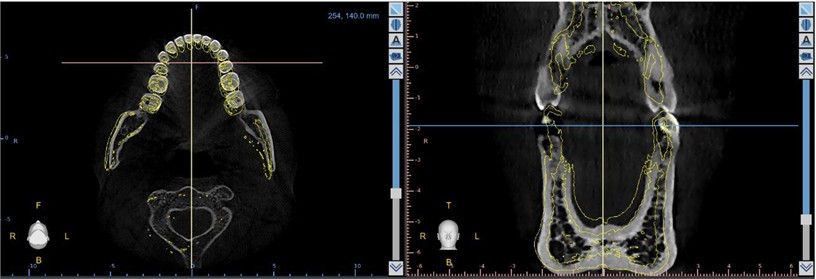
The remodeling of the basal and alveolar bone caused a passive teeth movement allowing the correction of malocclusion (Fig. 4). Inferior arch also suffered remodeling, equilibrating the transversal dimension (Fig. 5).
Fig. 4Teeth movement. The green line shows the original position of the teeth. On the right panel it is possible to visualize the vestibular shift of bone and of the first molar, correcting the crossbite showed on green line. Alveolar bone moved 0,77 mm and tooth crown 1,60 mm

Fig. 5Inferior arch remodeling. Yellow lines show the initial shape of the inferior arch and the original position of the teeth
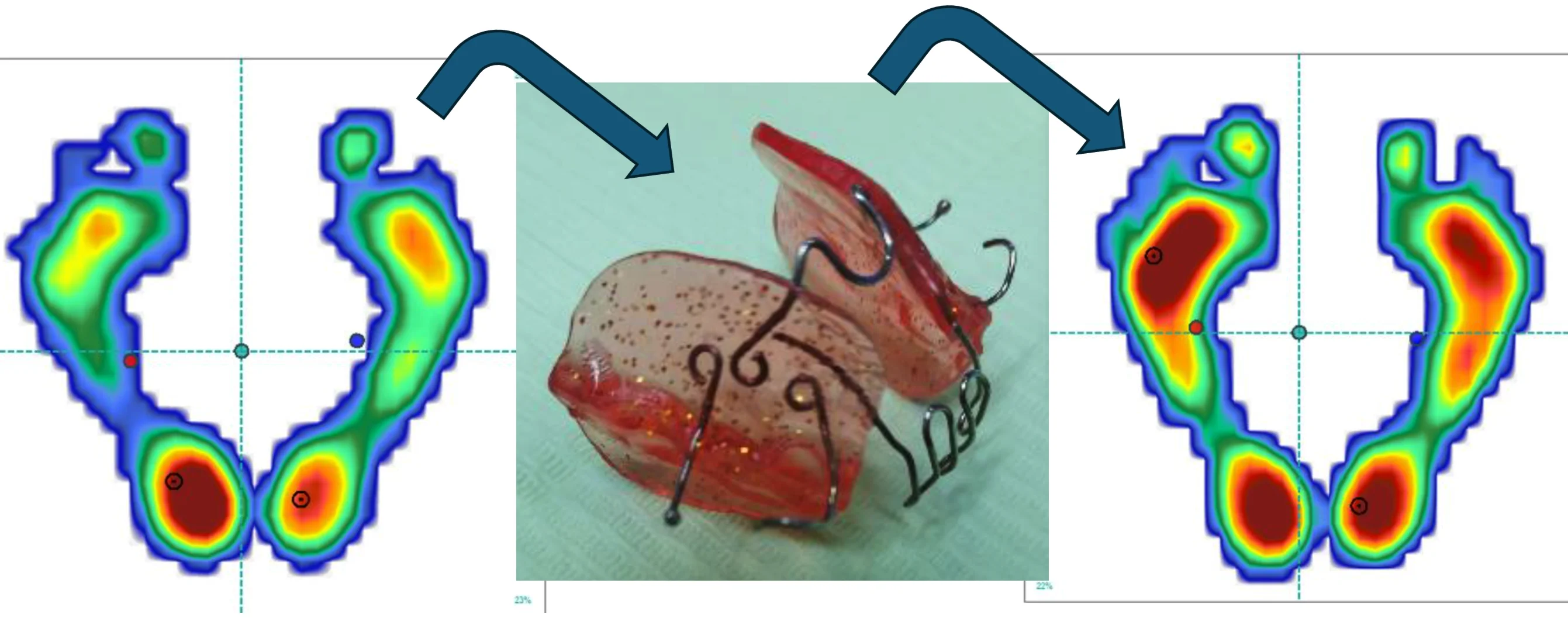
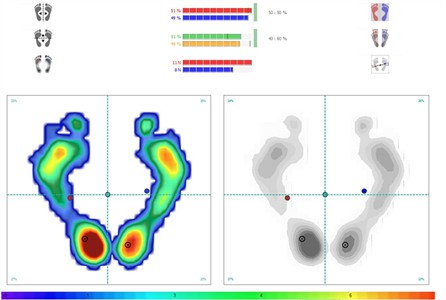
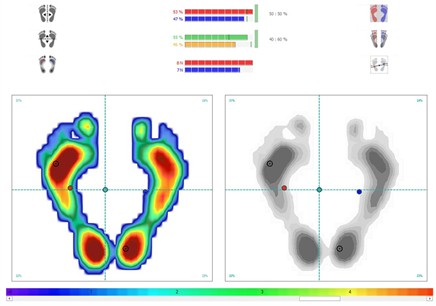
Body posture of patient was controlled during all treatment and showed great improvement as shown by DIERS (a compact and fast solution for a contact-free and synchronous 3D analysis of the body statics in order to detect malpositions) and baropodometry evaluation (Fig. 6 and 7).
Fig. 6DIERS. Posterior evaluation of posture. On left up beginning and on right up after treatment with CPB and manual therapy showing improvement Sagittal evaluation of posture. On left down, beginning and on right down after treatment and manual therapy showing significative improvement
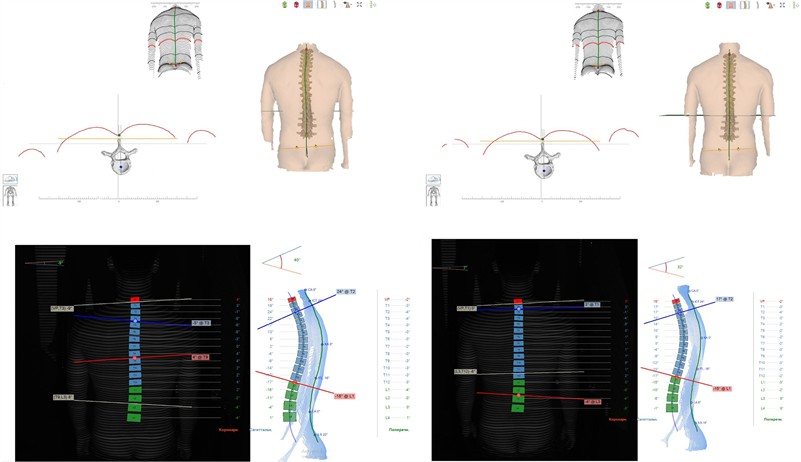
Fig. 7Baropodometer evaluation. On up panel the beginning register showing a body inclination to the crossbite side. On left the register after treatment showing a better posture balance
4. Discussion
Static and dynamic body postures are complex processes. For the correct establishment of posture, it is necessary the integration of afferences from the somesthetic, visual, vestibular and stomatognathic system. They will send to the central nervous system information to be decodified and generates efferences to adjust posture [7]. On this case, it is necessary to reinforce, that no mechanical force was used. Jaw functional orthopedics uses mandible and tongue posture changes to equilibrate the bone remodeling and, consequently, the occlusion, changing the proprioception information that will be sent to CNS [8]. In general, our result emphasizes the necessity of the integration of osteopathic and jaw functional orthopedic approaches to improve the results of the treatment and, consequently, the quality of life of patients.
5. Conclusions
CPB appliance is a functional appliance that follow the fundamental principles of Jaw Functional Orthopedics. It was effective on maintaining the tongue and mandible posture for the related case. It also stimulated the transversal growth of maxillae allowing a new postural engram observed on the DIERS registration and on the baropodometric exam.
References
-
D.C. Page, “How to promote and provide functional jaw orthopedics,” The Functional Orthodontist, Vol. 18, No. 1, pp. 22–30, Mar. 2001.
-
K. Yashiro, M. Takagi, and K. Takada, “Smoothness of chewing jaw movements in adults with mandibular prognathism,” Journal of Oral Rehabilitation, Vol. 39, No. 2, pp. 100–110, Sep. 2011, https://doi.org/10.1111/j.1365-2842.2011.02256.x
-
R. P. Knigge et al., “Craniofacial growth and morphology among intersecting clinical categories,” The Anatomical Record, Vol. 305, No. 9, pp. 2175–2206, Feb. 2022, https://doi.org/10.1002/ar.24870
-
W. A. Simões, Ortopedia Funzionale dei Macellari Attraverso la Riabilitazione Neuro-Occlusale. (in Italian), Italia: Orbetello, 2010.
-
“Method for diagnosing a person’s health when planning and conducting osteopathic functional dental treatment by doctor datsenko’s method,” RU2779362C1, 2022.
-
“Orthodontic-orthopedic device for cranial-postural balance Vasilyeva,” RU221179U1, 2023.
-
C. Ioniță, A. E. Petre, R.-S. Cononov, A. Covaleov, I. M. Brindusa, and A. S. Nica, “Methods of postural analysis in connection with the stomatognathic system. A systematic review,” Journal of Medicine and Life, Vol. 16, No. 4, pp. 507–514, Apr. 2023, https://doi.org/10.25122/jml-2022-0327
-
M. Bovi Corsi, “Successful balance of occlusal plane using functional orthopedics appliance,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 2, No. 2, pp. 107–114, Nov. 2022, https://doi.org/10.21595/jfocg.2022.22805
About this article
The authors have not disclosed any funding.
The authors acknowledge Dr. Grigory S. Perevezentse for helping on posture evaluation.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Maria Vasilyeva: conceptualization, data curation, formal analysis, investigation, methodology, resources, software, supervision, validation, visualization, writing-original draft preparation, writing-review and editing. Patrícia Valério: conceptualization, data curation, investigation, methodology, project administration, supervision, validation, visualization, writing-original draft preparation, writing-review and editing.
The authors declare that they have no conflict of interest.
Informed consent signed by the patient was obtained.
