Abstract
Temporomandibular joint (TMJ) ankylosis is one of the most disabling pathological conditions that can occur in the maxillofacial region, often occurring at an early age, limiting growth and causing facial deformity, which significantly affects the quality of life of the individual. The objective of the study was to evaluate the contribution of Jaw Functional Orthopedics (JFO) in TMJ ankylosis after the surgical phase. The case of a 7-year-old female patient diagnosed with bilateral condylar ankylosis (fibrous ankylosis on the right side and bony ankylosis on the left side) is presented. On clinical examination, facial asymmetry, retrognathia, muscle contraction and opening limitation were observed. Treatment consisted of temporalis muscle flap rotation surgery with condylectomy and coronoidectomy, physical therapy, and functional therapy with OFM. The clinical results at 4 months of follow-up suggest significant progress in oral opening and protrusion. The patient showed a high degree of satisfaction with the results obtained. She is currently continuing with the use of orthopedic appliances to correct the sequelae of ankylosis and improve mandibular kinematics.
Highlights
- JFO stimulates the functional movements of the mandible, favors its growth and promotes condylar repositioning and remodeling, helping the correct mandibular position.
- Its purpose is to keep the joint in continuous movement and stimulate maximum mouth opening, so its use in the treatment of TMJ ankylosis promotes better results.
- A comprehensive treatment protocol should be followed, including a surgical plan, physical therapy and functional orthopedics, in addition to periodic monitoring of its evolution, thus obtaining better long-term results and avoiding complications such as reankylosis.
1. Introduction
Temporomandibular joint (TMJ) ankylosis is classified as a disorder of chronic mandibular hypomobility, leading to partial or total limitation of jaw movements [1], [ 2]. It occurs due to a bony, fibrous or fibro-osseous fusion of the structures of the temporomandibular joint (TMJ) [3].
It is one of the most disabling pathological conditions that can occur in the maxillofacial region, as it affects the quality of life of the individual by interfering with speech, chewing, oral hygiene, facial and mandibular growth and esthetics [2], [4], [5] and can also lead to malnutrition and psychosocial repercussions [1].
This condition often occurs at an early age and limits growth, resulting in facial deformity and poor airway space [5].
There are several classifications of temporomandibular ankylosis (Rowe, Topazian, Shawney, the latter being one of the most widely used today) which depend on several factors: 1. By the location of the ankylosed tissue: intra-, extra- or juxta articular. 2. By the affected joints: unilateral or bilateral. 3. By its extension: partial or total. 4. By the degree of mobility it allows: hypomobile or immobile. 5. By the predominant type of tissue: fibrous, osseous or fibro osseous. 6. By the stage at which it presents: congenital (it is very rare and severe) or acquired [1], [6].
The clinical features vary in relation to the time of evolution, the age at which the process has started and whether the alteration is unilateral or bilateral. In the case of being unilateral there is limitation of the oral opening and facial asymmetry due to mandibular hypoplasia on the affected side; the chin is returned and deviated towards the affected side; the ipsilateral gonial angle is higher; occlusally there is inclination of the lower incisors towards the healthy side, crossbite on the affected side and inclination of the occlusal plane [2].
In the case of bilateral ankylosis, the posterior facial height decreases, retrognathia and limitation of oral opening appear, with some degree of shortening and hypertrophy of the masseter, pterygoid, temporalis and suprahyoid muscles, due to isometric contractions [2].
The most common cause is due to hemarthrosis secondary to trauma [1], [2] but it can also be due to autoimmune, infectious or congenital causes [1].
It mainly occurs due to trauma (especially in intra- and extracapsular fractures with dislocation of the condyle to a medial and anteromedial inferior level) and infectious processes (parotid abscesses, otitis media, suppurative arthritis, psoriatic arthropathy, osteomyelitis, among others), inflammatory and degenerative processes (ankylosing spondylitis, juvenile rheumatoid arthritis or Still’s disease), hemarthrosis, radiotherapy, burn synechiae, scleroderma, myositis ossificans, lead poisoning, prolonged interdento-maxillary fixation, intrauterine or perinatal trauma, among others [6].
For treatment it is ideal to use a comprehensive care protocol, which includes history taking and diagnosis, surgical therapy, early physical therapy and functional orthopedics of the jaws [7].
The surgical phase of TMJ ankylosis should include the interposition of some material into the space formed after performing the condylectomy. Such material may be autogenous or alloplastic so that recurrence is avoided.4 The most commonly used therapies are arthroplasty, en bloc resection of the bony segment, joint reconstruction, creation of a new joint using rotational or non-rotational flaps, and grafting [8].
A fundamental part of the treatment is functional therapy with braces, which should be started 24 hours after correction of the ankylosis. The therapy consists of opening, closing, lateral and protrusive movements. Subsequently, different appliances are used to correct sequelae, promote mandibular myofunctional development and achieve alignment of the dental arches [8], [9].
2. Clinical case
This study presents the case of a 7-year-old female patient from San Fernando de Apure, who came to the Hospital Militar Universitario ¨Dr. Carlos Arvelo¨, because she had a significant limitation of oral opening, her representative refers that the patient suffered a trauma of 8 meters high in 2018, she went to a medical service where she was indicated the use of a neck brace for the next 3 years.
Clinical evaluation showed retrognathia and muscle contraction, which was more accentuated on the left side and a 1,5 mm mouth opening (Fig. 1).
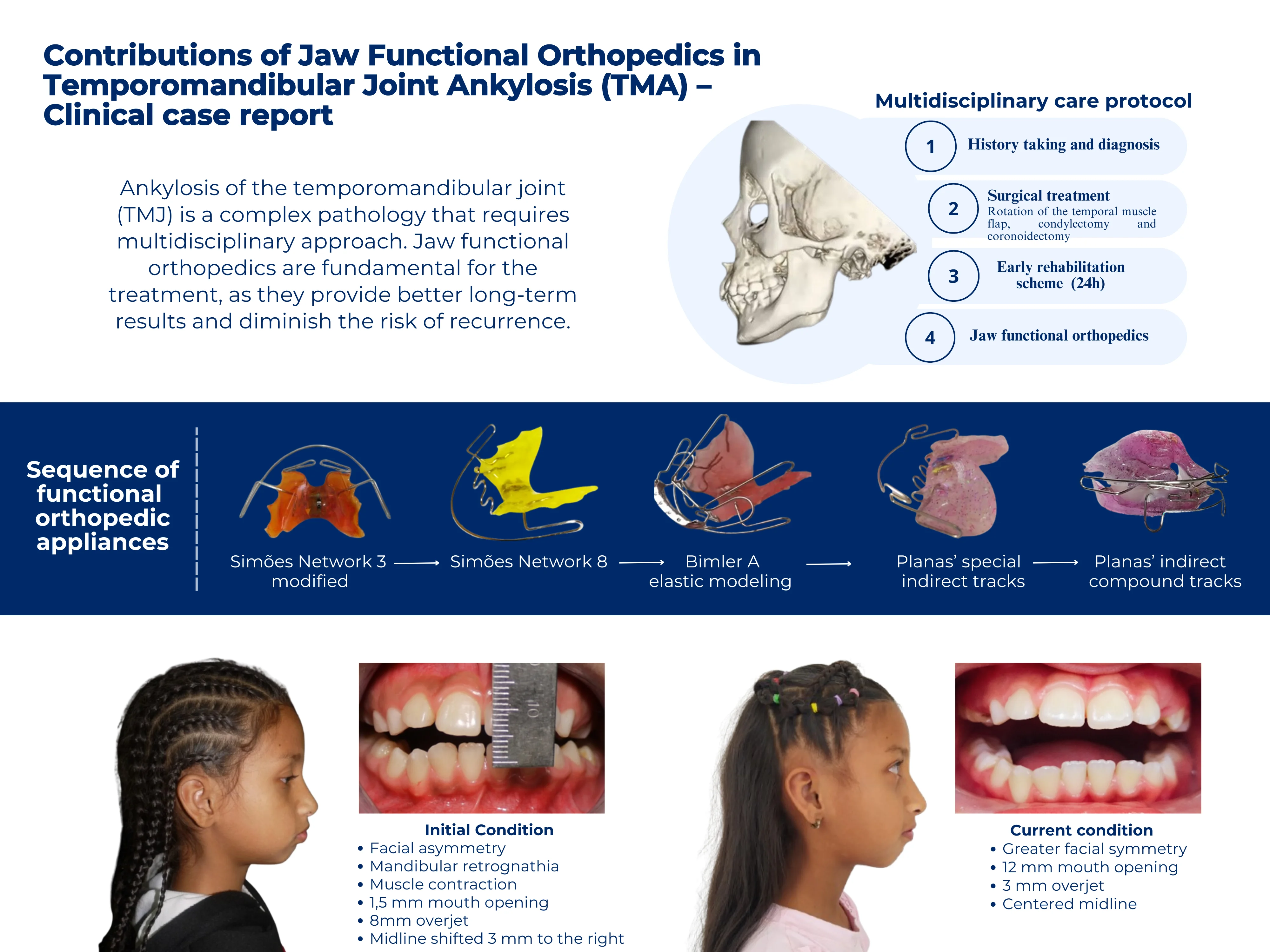
In the tomography, bone ankylosis is observed and coronoid hyperplasia is presumed on the left side, in addition the deepening of the antegonial zone is appreciated on both sides of the mandible (Fig. 2).
After studying the case, the patient was diagnosed with bilateral condylar ankylosis (fibrous ankylosis on the right side and bony ankylosis on the left side).
Fig. 1a) Mouth opening 1,5 mm, b) frontal facial view, asymmetry, c) right lateral facial view, mandibular retrognathia, d) left lateral facial view, muscle contraction. Image courtesy: Od. S. Siverio, and Od. M. Carreras. Residents of the postgraduate course of Maxillofacial Surgery of the University Military Hospital ¨Dr. Carlos Arvelo¨

a)

b)

c)

d)
For this type of patients, a 4-step care protocol is applied, consisting of: 1. History taking and diagnosis 2. Surgical treatment, 3. Rehabilitation scheme and 4. Functional orthopedics [7].
As the first phase of the treatment, the surgical procedure was performed, this is based on eliminating the ankylotic part, reestablishing the articular function and above all preventing the reankylosis of the TMJ, for this it is necessary to use an interposition material after the arthroplasty [10], which was done by means of the rotation of the temporal muscle flap, accompanied by condylectomy and coronoidectomy. After surgery, a 6 mm buccal opening was achieved.
Fig. 23D reconstruction cranial computed tomography. Image courtesy: Od. S. Siverio, and Od. M. Carreras. Residents of the postgraduate course of Maxillofacial Surgery of the University Military Hospital ¨Dr. Carlos Arvelo¨
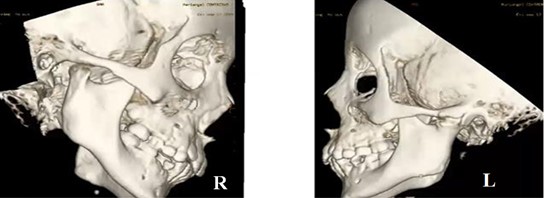
Fig. 3Surgical procedure. Image courtesy: Dr. Jose Gregorio Melillo. Buccomaxillofacial surgeon.

The aim of the surgical treatment is to restore mandibular mobility and improve growth to reduce the possibility of facial asymmetry in the future [10] and improve the patient’s quality of life, however, it is important to note that when the girl’s growth stage is completed, she must undergo another surgical procedure to place a TMJ prosthesis.
After surgery, the rehabilitation scheme begins with immediate physiotherapy after 24 hours, when postoperative pain has decreased, opening and closing movements are performed for 20 minutes four or five times a day, lateral and protrusive movements should also be performed in a forced manner with the help of a family member, to avoid reankylosis. However, these movements in the patient were very limited.
Manual therapy is also performed at muscular level to maintain a state of relaxation of the muscles involved in the opening and closing of the mandible, this should be accompanied by heat therapy. In addition, the patient and her representative were educated to perform these exercises at home.
Simultaneously, treatment with Functional Orthopedics of the Maxillae was started. Fig 4 shows the extraoral images where the post-surgical conditions can be appreciated.
Fig. 4Post-surgical condition: a) frontal facial view, asymmetry, b) frontal facial view smiling, c) right lateral facial view, d) left lateral facial view

a)

b)

c)

d)
Firstly, a sectioned Simões Network 3 (SN3) was placed, since the limited mouth opening did not allow the use of the original appliance, with this, the bite was slightly lifted, the intention was to achieve a change of posture, lateral, protrusive and lateropropulsive movements. The following week, a slight bite lift and alignment of the teeth to the midline is already visible, as shown in Fig. 5(e). This appliance remained in the mouth for 2 weeks.
Fig. 5Intraoral condition: a) Simões Network 3 sectioned, b) frontal intraoral view, c) lateral intraoral view, increased overjet 8 mm, d) deviated midline before SN3, e) centered midline after SN3

a)

b)

c)
d)

e)
Despite the slight increase in buccal opening achieved with the previous appliance, the opening was still very limited and did not allow taking a lower impression, so it was decided to place a Simões Network 8 (SN8), in order to achieve mandibular advancement and protrusion movements, this appliance, despite being anchored in the maxilla, has important effects on the mandible.
Fig. 6a) Simões Network 8 (SN8), b) lateral view with SN8, c) 12 mm buccal opening

a)

b)

c)
At this stage of the treatment, we were able to increase the buccal opening to 12 mm and achieve a protrusive movement of 3 mm (Fig. 6(c)). This device remained in the mouth for 2 months.
To this point, the buccal opening of the patient allowed taking the inferior impression, so a Bimler A elastic modeling could be performed. According to Bimler his modelers are governed by the patient's own nervous and reflex elements. The modeler performs expansion to a certain degree and then terminates automatically when equilibrium is achieved [11]. With the use of this device, facial changes were observed, as well as greater symmetry and the mouth opening was maintained (Fig. 7(c)).
Fig. 7a) Bimler A elastic modeler, b) front view with Bimler A, c) mouth opening, d) frontal facial view, greater symmetry, e) lateral facial view
a)

b)

c)

d)

e)
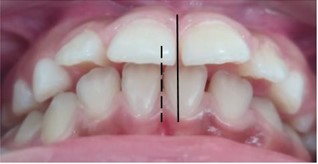
Nine months later, the patient came back for consultation, and it was decided to place Planas’ special indirect tracks in order to make the mandible slide and generate lateral and protrusive movements, in addition to improving the proinclination of the anterosuperior teeth (Fig. 8).
Fig. 8Planas’ special indirect tracks


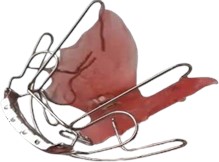
Fig. 9Planas’ indirect compound tracks


The following month, the proinclination of the anterosuperior teeth had improved, achieving an overjet of 3 mm, which is within normal parameters, and a protrusive of 3 mm.
Therefore, it was decided to change the appliance for Planas’ indirect compound tracks (Fig. 9), which establish a physiological occlusal plane with freedom of movement and rehabilitatesn the TMJ, providing a system in harmony with maximum performance and minimum effort [12].
3. Results
Among the results that can be quantified are the increase of the buccal opening, the decrease of the overjet and the centering of the dental midlines (Table 1). On the other hand, we were able to improve mandibular kinetics since the patient is able to perform movements in all planes of space, achieving a stable and harmonious system, avoiding reankylosis.
Table 1Results
Initial condition | Immediate Post Surgical - May 2021 | June - September 2021 | September 2021 - July 2022 | |
Orthopedic appliances | None | None | SN 3 SN8 | Bimler A Planas’ tracks |
Buccal opening | 1,5 mm | 6 mm | 12 mm | 12 mm |
Overjet | 8 mm | 8 mm | 8 mm | 3 mm |
Midline | Offset 3 mm to the right | Offset 2 mm to the right | Centered | Centered |
4. Discussion
The functional orthopedic appliances of the jaws stimulate the functional movements of the mandible favoring its growth, promoting condylar repositioning and remodeling, thus helping the correct position of the mandible [14].
By means of the Simoes Network a change of therapeutic posture is generated, they act directly on the neuromuscular system, generating specific effects, such as increasing lateroprotrusive movements, changes in the position of the tongue, among others [15], [16].
On the other hand, the Bimler elastic modelers provoke reflex muscular reactions in sagittal, transverse and vertical directions and activate the total function of the matrix for therapeutic tasks. These devices generate an advanced position of the mandible [17].
The Planas’ tracks stimulate laterality movements, improve mandibular propulsion and vertical growth of the affected limb, thus leveling the occlusal plane. In addition, it improves facial asymmetry and the dental midline. On the other hand, the literature reports the use of orthopedic appliances, such as Planas’ tracks, Bionator, Twin Block, Frankel [9] and Spring Bite for the correction of sequelae caused by ankylosis [9], [13].
This form of action should create new postural reflexes and other mandibular dynamics, which produce and maintain the harmony of the stomatognathic system and thus correct masticatory efficiency [16].
The use of these appliances is extremely important to avoid post-surgical complications, such as TMJ reankylosis, which has a high recurrence rate, a condition that is evidenced in the study by Ramly E. et al. where the entity recurred in 75 % of the cases [18]. Although there are several known factors that could contribute, a greater recurrence has been associated with cases where the use of functional appliances is not implemented in the postoperative therapy [20].
In the same context, Belmont F. et al. describe the use of OFM in postoperative temporomandibular ankylosis, which favors mandibular myofunctional development and prevents reankylosis [9].
The purpose of these appliances is to keep the joint area in continuous motion and to stimulate maximum mouth opening [20], so they play a key role in predicting more favorable outcomes following surgical therapy of TMJ ankylosis.
5. Conclusions
The clinical course and management of patients with TMJ ankylosis is complex and typically involves a high recurrence rate [18].
It is therefore important to care for these patients in a comprehensive manner, applying a protocol that includes everything from a surgical plan, physical therapy and functional orthopedics. In addition to periodic follow-up of their evolution, thus obtaining better long-term results and avoiding complications such as reduced aperture, reankylosis, functional, nutritional and esthetic sequelae.
As evidenced in this case, OFM represents an important contribution in the treatment of TMJ ankylosis since it generates stimulation of mandibular movements within physiological limits and prevents the recurrence of this condition. However, scientific evidence on this subject is scarce, so further research is suggested.
References
-
V. D. Cázarez-Ríos, J. Téllez-Rodríguez, and R. López-Fernández, “Temporomandibular ankylosis in pediatric patients,” (in Spanish), Mexican Journal of Pediatrics, Vol. 87, No. 5, pp. 189–194, Jan. 2020, https://doi.org/10.35366/97173
-
D. Molina, P. Aguayo, C. Ulloa, V. Iturriaga, T. Bornhardt, and M. Saavedra, “Ankylosis of the temporomandibular joint: A review of the literature,” (in Spanish), Advances in Odontostomatology, Vol. 29, No. 5, pp. 239–244, Oct. 2013.
-
H. Bénateau, A. Chatellier, A. Caillot, D. Diep, J.-D. Kün-Darbois, and A. Veyssière, “Temporomandibular ankylosis,” (in French), Journal of Stomatology Maxillofacial Surgery and Oral Surgery, Vol. 117, No. 4, pp. 245–255, Sep. 2016, https://doi.org/10.1016/j.revsto.2016.07.001
-
N. Atilas, M. Costa, P. R. Dominguete, D. Andrade, R. Generoso, and A. Ribeiro, “Unilateral mandibular condylar ankylosis – clinical case report,” (in Spanish), Venezuelan Dental Act, Vol. 46, No. 2, pp. 187–190, Jun. 2008.
-
N. Mittal, M. Goyal, D. Sardana, and J. S. Dua, “Outcomes of surgical management of TMJ ankylosis: A systematic review and meta-analysis,” Journal of Cranio-Maxillofacial Surgery, Vol. 47, No. 7, pp. 1120–1133, Jul. 2019, https://doi.org/10.1016/j.jcms.2019.03.029
-
E. González and A. Hernández, “Temporomandibular ankylosis. Literature review. Management protocol and case report,” (in Spanish), Official Journal of the Mexican Dental Association, Vol. 64, No. 6, pp. 238–243, 2007.
-
S. Siverio and M. Carreras, “Treatment protocol of Temporomandibular Joint Ankylosis (TMJ) in pediatric patients,” (in Spanish), University Military Hospital Dr. Carlos Arvelo, Caracas, Venezuela, 2023.
-
E. Vite-Vera, H. Zúñiga-Domínguez, L. Moreira-Cedeño, C. Escala-Parker, C. Rivera-Salas, and R. Marín-Ferrín, “Ankylosis of the temporomandibular joint,” (in Spanish), Cuban Journal of Rheumatology, Vol. 21, No. 3, 2019.
-
F. Belmont-Laguna, L. Sánchez-Matus, J. Téllez-Rodríguez, and H. Ceballos-Hernández, “Functional therapy in postoperative temporomandibular ankylosis in pediatric patients,” (in Spanish), Pediatric Act of Mexico, Vol. 28, No. 3, pp. 111–117, 2007.
-
D. Cebreros Rosas, “The temporalis muscle flap in TMJ surgery: is it still a valid option?,” (in Spanish), Spanish Journal of Oral and Maxillofacial Surgery, Vol. 44, pp. 63–69, Jan. 2022, https://doi.org/10.20986/recom.2022.1354/2022
-
C. Lobo and C. Medina, “Orthopedic treatment in pediatric patients with a history of condylar fracture,” (in Spanish), Central University of Venezuela, Caracas, Venezuela, 2005.
-
P. Planas, Neuro-Occlusal Rehabilitation. (in Spanish), 2013.
-
C. Acosta Behrends and G. Loranca Fragoso, “Hyperplasia of mandibular coronoid processes: a new postsurgical treatment,” (in Spanish), Spanish Journal of Oral and Maxillofacial Surgery, Vol. 37, No. 2, pp. 93–98, Apr. 2015, https://doi.org/10.1016/j.maxilo.2013.11.001
-
A. Olaya and M. Padilla, “Orthopedic management of temporomandibular dysfunction in children: review of the literature,” (in Spanish), Colombian Dental Act, Vol. 6, No. 1, pp. 163–175, 2016.
-
O. Quirós, Manual of Functional Maxillary Orthopedics and Interceptive Orthodontics. (in Spanish), Colombia: Latin American Medical and Dental News C.A., 1993.
-
W. A. Simões, “Functional orthopedics of the jaws and open bites,” (in Spanish) in Update in orthodontics and functional orthopedics of the jaws, São Paulo: LTA Medical Arts Editor, 2002.
-
H. P. Bimler, Bimler – Elastic modelers and compact cephalometric analysis. (in Spanish), Caracas: Latin American Medical and Dental News C.A., 1993.
-
E. P. Ramly et al., “Temporomandibular joint ankylosis in pediatric patients with craniofacial differences: causes, recurrence and clinical outcomes,” Journal of Craniofacial Surgery, Vol. 31, No. 5, pp. 1343–1347, Mar. 2020, https://doi.org/10.1097/scs.0000000000006328
-
H. Behnia, M. H. K. Motamedi, and A. Tehranchi, “Use of activator appliances in pediatric patients treated with costochondral grafts for temporomandibular joint ankylosis: Analysis of 13 cases,” Journal of Oral and Maxillofacial Surgery, Vol. 55, No. 12, pp. 1408–1414, Dec. 1997, https://doi.org/10.1016/s0278-2391(97)90639-x
-
L. Barroeta, “Fractures of the mandibular condyle in pediatric patients,” (in Spanish), Central University of Venezuela, Caracas, Venezuela, Thesis Specialty, 2023.
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ivonne Duran was responsible for oversighting and leadering the research activity planning and execution, as well as clinical management of the patient and execution of treatment with functional orthopedic appliances. Adrimar Cano was responsible for conducting a research and investigation process, as well as the original draft preparation creation and/or presentation of the published work, specifically writing the initial draft (including substantive translation). Paola Gil was responsible for conducting a research and investigation process and revision and editing of the article.
The authors declare that they have no conflict of interest.
The research met all applicable standards for the ethics of experimentation. The representative gave written informed consent prior to the study.
