Abstract
Relapse has always been the main problem in orthodontics. But is it due to the treatment method? Or the age of the patient or the anatomy of the skull? At the examples of some case histories, these questions are considered and hopefully, will contribute a bit to this eternally controversial subject.
1. Introduction
Killing time in the waiting room of a doctor’s office, I re-read an old publication “Treatment of Anterior Open Bite with the Bimler Functional Appliance: Report of Three Cases” by Ramirez-Yañez et al. Besides two basic mistakes on the first page (The mistakes: No need for a new appliance every 6-8 months, you simple adjust the wires of the old one. And no need for 24 hrs. as night time wear is fully sufficient), what a nice surprise: It praised my father’s appliance, furthermore I appear as co-author [1].
This was thanks to the case reports of my father’s clinic, with long-term follow-up. But to say the truth, alas, the wonderful long-term stability is not-only! – due to the wonderful Bimler appliance but mainly to two conditions: The “harmonious” skeletal features and a respective treatment goal.
2. Harmony
“Harmony” as a main topic of the Bimler Cephalometric Analysis came up only recently, as a friend asked if it had any connection with “biotype”. I had never heard of biotype in my life. My father had something quite different in mind than “organism sharing the same genotype”. His “harmony” concept as opposed to norm values is quite simple, which he was very proud about.
Looking at the occlusion, there are three skeletal units involved: of course, mandible and maxilla, and as importantly the temporal bones. Not for nothing, they give name to and house the temporomandibular joints which are the connection of the two other units, mandible and maxilla. This third party, often overlooked, plays a prominent role in the sagittal relation. And naturally, as our two old friends maxilla and mandible grow in the growing child, so do the temporal bones, carrying the joints plus mandible backwards in relation to the maxilla. Usually, this is more than compensated for by the mandibular growth. But these three components of the occlusion are passed on independently from each other, from father’s or mother’s side. Still, it makes no difference if the inherited bones are large or small, as long as they are all of them large or small. When an unlucky child gets badly matching bones, it might become a case for a facial surgeon. Thus, the idea of a “norm” size becomes irrelevant, important is the inherited inherent harmony. “Harmonious” orthodontic patients have a good prognosis no matter what treatment system is employed and usually do not need retention.
This applies basically to the sagittal relation. These three simple linear measurements are sufficient:
– Depth of maxilla A to TV (Tuber-Vertical).
– Joint position TV to point C (center of head of condyle).
– Diagonal length of mandible.
The results are grouped as small, medium and large. Nobody would call one size more “normal” than another, just like with T-shirts. In different countries, the values can be adapted to the local population, as Dr. Mikiko Nagai from Nagano, Japan, does for her patient load.
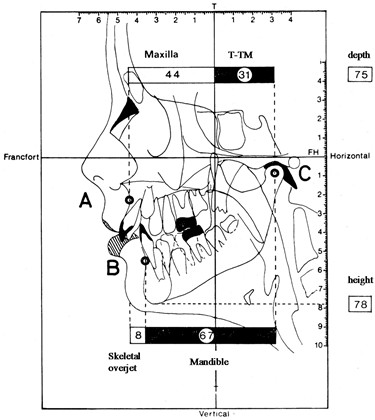
Fig. 1Three linear measurements as proposed by Bimler 1961. From: Lineare Messungen am Fernröntgenbild, Fortschr. Kieferortho,36, 1975, p. 36. (The linear measurement approach goes back to Wendell L. Wylie, (1913-1966) an American orthodontist who served as a President of American Board and the Chief Editor for The Angle Orthodontist Journal.) Here, the three measurements are supplemented by the „Skeletal Overjet” = point A to point B, the skeletal sagittal relation
3. Prognosis
With the help of this system, the doctor can give a rather decent prognosis for the outcome and stability of his respective patient. Of course, it is true that not every prognosis becomes true, especially under functional treatment. Who is to blame? The dentist will blame the patient for non-compliance, and the patient will blame the dentist for incapability. More often it is simply bad luck with a bad growth pattern which usually is inherited. It can also be acquired during pregnancy maybe by drugs or medicine taken by the mother. Maybe it is something like a mini syndrome of a cleft lip. The most common growth impediment affects the maxillary bone which then shows a three dimensional under development, leading to a straight profile, ectopic canines, maybe a frontal open bite etc. It is a rather common phenomenon which makes the person even look quite pretty, as the small nose gives a juvenile appearance. It is often combined with mouth breathing, and the open bite can be quite relapse-prone. On the other hand, a “functional” open bite will close almost by itself as soon as the finger or tongue are kept away. Obviously, stability depends a lot on the skeletal conditions. As the inclination of the nasal floor is a good indicator for this problem, additional angular measurements are here very useful.
4. Functionalism
My father was a medical doctor, he worked as a physician during the war and also in the British captivity afterwards. His father was a dentist, who had to leave his home town in the far east of Germany, today Poland, fleeing from the Red Army to the American occupation zone. My father’s dream was to become a facial surgeon.
However, after the war, there were very many surgical doctors dealing with facial injuries but hardly any dentists as they had not been so urgently needed for the last couple of years. The new government offered to doctors of medicine the license as dentist after only three trimesters, nine months of studies. My father made it in six months, as he often proudly mentioned. Of course, thus he hardly knew a thing about dentistry, and his approach to orthodontics was rather medical.
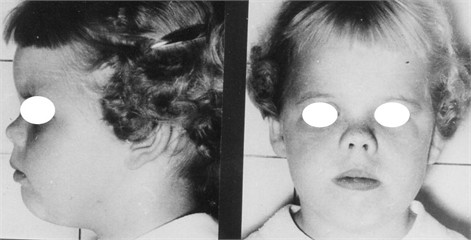
Fig. 2The Micro-rhinic Dysplasia. First published in Revista Española De Estomatologia, Vol. 14, No. 4, 279-303, Barcelona 1966. English translation 2012 by A. B. Bimler, in: Jaw Functional Orthopedics and Craniofacial Growth, 2024
Functional treatment generally is only popular in countries where dentistry was historically a specialization of medicine with a more “holistic” look not only at the teeth but at the surrounding tissue. Fully in accordance with the medical tradition of checking the patient’s response like with a fever curve, Bimler used a “reaction curve” to check thew efficiency of his new appliance. He had to develop an appliance himself because as a refugee in the economic postwar difficulties, he could not effort to purchase the material for any other. The money was there only for wire and maybe some little acrylic. His regular measurement of the patient’s arch widening also showed him the pointlessness of the Pont Index, another norm value. In fact, he saw to his surprise the different speed and amount of the reactions to the same appliance. He learned that this was not due to compliance. He learned that night-time use only had the same results like all-day use. Of course, it disappointed him a bit, as he had been very proud that his slim, graceful appliance could comfortably be worn all day long as opposed to the clumsy Bionator.
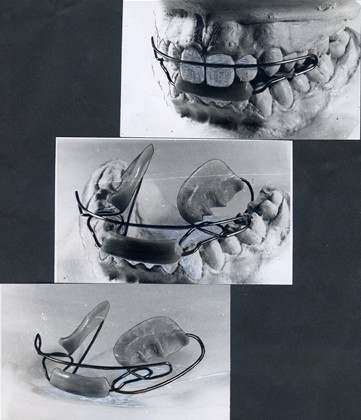
Fig. 3Historic Bimler A-type appliance. This photograph from the late 19540 shows a prototype of the Bimler Appliance, still without the Coffin Spring and with the “cap” of the activator. This would later be replace by the frontal splint and the lingual loop to guide the mandible forward, at the same time securely avoiding an unwanted protrusion of the lower front
5. Failure
But why were there the failures and “bad” patients? The ones who needed extractions? Who was to blame? About one third of the patients had not fully satisfying results. During his medical career, he had worked also in an ENT-office, and now he remembered that about the same number of the tonsillectomy cases stayed mouth breathers, though the surgery had been performed correctly. Trying to look at problems from a fresh angle, he started to study not the tissue but the empty hollow spaces, the airways. In 1954, his first publications about x-ray studies carries the title: x-ray presentation of the upper airways [2]. In the “conclusion” he writes: There are two groups of pathologic narrowing of the upper airways. One is a hypertrophy of the lymphatic tissue and reacts well to an operation. The other is a skeletal growth impediment of the mid face, and tonsil removal cannot solve the problem of mouth breathing. It affects over 20 % of the patients [3].
This ratio roughly coincides with his own observation on arch widening. Of course, an underdeveloped maxillary bone would not only constrict the airways but also cause crowding of the teeth like ectopic canines. As the skeletal under-development would sometimes be unilateral, and the ectopic canine unilateral, he supported consequently unilateral extractions. About the dentists’ ideal of midline and Class-I molar occlusion, he said that they were dentist’s ideas and the patients were not even really aware of them.
6. Treatment
Accordingly, the final treatment result would not be decided by the dentist but the patient’s reaction, his intrinsic body-feedback and responses to the functional treatment. How could that work? The elastic removable appliance has a “chewing-gum effect”, it is causing constant mandibular movements and, due to the increased saliva flow, constant swallowing. By these movements, the wires would touch and un-touch the teeth and move them by intermittent force –causing significantly less root resorption [4]. After an activation, if the therapeutic force is too strong and the appliances does not feel comfortable, the patient, also during the sleep, will remove or “loose”, as they call it, and thus absolutely avoid any iatrogenic damage to the surrounding tissue or the joints. The patients will return to the office where the dentist de-activates the appliance always asking: “Is this correct now, does it feel comfortable?”, and even very young children can answer this question correctly. Consequently, there are hardly any compliance problems with the Bimler. We never have a gum problem or joint pain.
7. Finishing
When the limits of the functional non-anchored treatment, controlled and guided by the patient’s intrinsic body-response, were reached, the results look often enough to critical eyes as unfinished. When, now as a second step, the dentist-controlled, fixed treatment starts, it will be a much easier job in much shorter time on the best possible “natural” base. The damaging side effects will be less and the retention easier respectively the relapse less noticeable. Finishing is certainly the week point of functionalism, and in the end, the customer pays and is king. Teenagers are understandably more interested in present cosmetic looks than in long term side effects.
8. Age
All life long, the teeth respond to pressure or traction and change their position accordingly. That does not mean that all ages were as good as another for functional treatment. Even if a long-term influence on the basal bone shape remains questionable today, there is always the alveolar bone. This one necessarily must adapt to many changes during the change of teeth, and this is the chance to lastingly influence it by orthodontic treatment, especially in the problematic vertical dimension.
The study of open-bite cases which made me a “co-author” of the above-mentioned publications by Ramirez-Yañez, all treated the same way with a Bimler A-Type appliance, showed a good long-term stability if the treatment was started before 10 years of age. A later start also produced nice results, but after 30 years, a certain relapse was obvious. The same seems true for deep-bite cases, which are very nicely responding to the Bimler-A-Type for mixed dentition with a beautiful stability and in adults, to the Bimler B-Type, but those need permanent retention afterwards. Usually, it is enough to use the “functional retention” wearing the very light Bimler zero-type one night every week. Alas, once the permanent teeth are in place, the alveolar bone does not adapt vertically so nicely anymore. Of course, the lowering of the bite at a certain age, over about 40 years, cannot be avoided but can probably be stopped or slowed down by the “functional retention”, using a simple Bimler A-0 Type once a week. But we do not have enough cases to give a solid opinion.
9. Old age
60 years ago, my father’s office was about the only one in our town, and many people my age, around 70 and older now, were his patients. As I kept my maiden name, they recognize it and ask: “Maybe you know this Bimler orthodontist?” And then I interview them a bit, if they still have their own teeth? And they all do, maybe with exceptions of some wisdom teeth. Nobody has an American president smile, though. They are all pleased because they have neither any implants nor joints pains.
Where do the joints come in? That is another point from the edges of dentistry: the Curve of Spee. This is in its original version [5] a circle that runs through the occlusal surface of the molars and touches the anterior part of the head of the condyles. It is a distinguishing feature of most mammals. Molars are called such because their task is to grind the food, from Latin molare = to mill or to grind. Like any millstone, grinding the food requires a circular surface for the grinding movement. There are exceptions like the mammals with a split upper lip, for example the hare or the camel who chew sidewise, and the ones who do not grind their food like dogs and cats. (So far, my ongoing research.) In English speaking language and orthodontic practice, the Curve of Spee means something different and gets flattened anyhow. Accordingly, the original version from 1890 is not talked much about. It seems possible, however, that any interference in this circle like flattening would either relapse or on the long run damage the joint, as the weakest player.
A removable appliance without anchorage cannot influence this physiological pattern, and my unrepresentative unscientific research on the long-term effect so far seems to detect only happy healthy patients half a century post-treatment. But the other ones probably would not talk to me anyhow.
Unfortunately, the long-term stability of a “beautiful” occlusion depends to a great deal on the inborn facial harmony of the patient.
10. Historical references on stability
Of course, we have all been aware of these problems, probably for 100 years now. I might quote Richard R. Riedel [6] who, in 1960, quotes Albin Oppenheim [7] “Retention is the most difficult problem in orthodontia”. Of course, this did not make the author very popular. Maybe it helps looking at another famous orthodontist who was at home on both sides of the Atlantic, Coenraad Frans A. Moorrees (1916-2003, whom I always admired not only for his superior intelligence but all the double letters in his name). He gave me the idea that it is a question of fixed versus functional and removable treatment. He talks about the concept of norm, like the “normocclusion” after Angle, which requires fixed treatment. Only a scope of the norm would lead to a more realistic treatment goal: “The norm is different in each single case” and “The average profile is only a useful abstraction”. He pleads for the individual treatment plan [8]. Of course, the “more realistic” the treatment goal, the better the stability. He and Riedel agree, however, that “the stability of the end results is one of the prime objectives” [6].
Moorrees and my father were born and died in the same years; Oppenheim (1875-1945) was forty years older. All three had a European education and war time background, which might explain their lesser approach towards perfection and a more “realistic” worldview.
Today in spring of 2025, an orthodontic teaching institute started his new advertising with the words: “Dear Doctor, finishing in orthodontics is not merely the final stage of treatment. It is the art of creating perfect occlusion, a harmonious smile, and long-term stability of results”. Long term stability remains a point of interest.
References
-
B. Bimler and D. Mahony, “Treatment of anterior open bite with the bimler functional appliance: report of three cases,” Dentistry, Vol. 4, No. 8, Jan. 2014, https://doi.org/10.4172/2161-1122.1000250
-
H. Peter Bimler, “X-ray imaging of the upper airways,” (in German), Fortschritte der Kieferorthopädie, Vol. 15, No. 3, pp. 206–213, Sep. 1954, https://doi.org/10.1007/bf02169948
-
H. P. Bimler, “In memoriam. about the micro-rhinic dysplasia,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 4, No. 1, pp. 63–74, Jun. 2024, https://doi.org/10.21595/jfocg.2024.23983
-
N. Ozkalayci, E. I. Karadeniz, S. Elekdag-Turk, T. Turk, L. L. Cheng, and M. A. Darendeliler, “Effect of continuous versus intermittent orthodontic forces on root resorption: A microcomputed tomography study,” The Angle Orthodontist, Vol. 88, No. 6, pp. 733–739, Nov. 2018, https://doi.org/10.2319/012518-68.1
-
F. C. Spee, “The displacement path of the lower jaw on the skull,” (in German) in Archives of Anatomy and Physiology, 1890, pp. 285–293.
-
R. A. Riedel, “A review of the retention problem,” Ange Orthodontiast, Vol. 30, No. 4, pp. 179–199, 1960.
-
A. Oppenheim, “The crisis in orthodontia,” International Journal of Orthodontia and Dentistry for Children, Vol. 19, No. 12, pp. 1201–1213, Dec. 1933, https://doi.org/10.1016/s0097-0522(33)90477-3
-
Moorrees and C. F. A., “Orthodontics in the United States of America in 1955 and 1956,” (in German), Fortschritte der Kieferorthopädie, Vol. 20, No. 1, pp. 86–101, Mar. 1959, https://doi.org/10.1007/bf02169331
-
A. Elie, “The See curve – orthodontics and reality,” (in German), ZWP online, Feb. 2011.
-
H. P. Bimler, “The importance of facial structure in open bite,” (in Spanish), Revista Española de Ortodoncia, Vol. 24, No. 2, pp. 153–167, 1994.
-
H. P. Bimler, “Phenomenology and analytics of therapy-resistant open bites,” (in German), Fortschritte der Kieferorthopädie, Vol. 49, No. 2, pp. 218–228, Mar. 1988, https://doi.org/10.1007/bf02163380
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The author declares that they have no conflict of interest.
The author declares that she is the daughter of the mentioned H. P. Bimler (1916-2003).
